
CMC Head, WuXi Vaccines
Recombinant protein vaccines, which are obtained by conventional genetic engineering, are based on the proteins of target pathogens that can activate our immune systems.
Unlike other types of vaccines that use viral genetic codes or viral vectors, recombinant protein vaccines use only the antigenic proteins themselves. This means that they cannot cause disease and that they generally do not need to be frozen for storage.
Their efficacy, intrinsic clinical safety, easy storage, and industrial production scalability have already positioned recombinant protein vaccines as the leading human vaccine technology. Today’s challenge is to make them as quickly, efficaciously, and cost-effectively as possible if they are to outpace new viral threats emerging in all corners of the world. Rethinking the production system for vaccines, with a view to shortening the time it takes for them to reach patients, could be the key to being better prepared for future health crises.
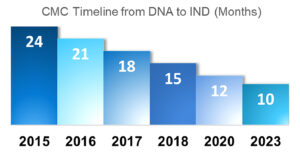
For example, as a result of the pressures placed on the industry during the COVID-19 pandemic to provide vaccines at an unprecedented rate, timelines have already changed. The graph in this article shows the evolution of monoclonal antibody (mAb) timelines since 2015, and similar patterns have been seen with other recombinant proteins used for vaccines. While a typical CMC timeline from DNA to IND application in 2015 would have been approximately 24 months, by 2023 the same pathway was expected to take only 10 months.
It is now broadly acknowledged that hastening the pathway from vaccine discovery to commercialization is not just desirable—it is an achievable step in our preparations to defend humanity against future pandemics. In recognition of this, the Coalition for Epidemic Preparedness Innovations (CEPI) has set an aspirational 100-Day Mission to make a safe and effective vaccine against any virus. This would give more people much faster access to more effective vaccines against a broader spectrum of infectious diseases. However, such achievements can only be achieved by leveraging technical strengths, CMC, regulatory capabilities, technical platforms, and commercial facilities.
Automated impact
A common challenge with recombinant protein vaccines is selection of the right antigen, requiring development of multiple antigens in parallel, or the product might be subjected to long development cycles. Such challenges may be tackled by applying advanced technology platforms.
In particular, a number of technologies now provide sufficient data to drive the change from manual to automation, and this can have a meaningful impact on the speed of vaccine development. For example, applying automation and digitalization to high-throughput process development and in-process testing platforms results in a faster and more systematic approach to purifying and verifying process samples, troubleshooting, and process optimization.
Automated liquid handlers can drive greater productivity, streamlined workflows and optimized assay precision and consistency, while automated buffer exchangers and customizable automated workflow equipment can give scientists access to high-throughput end-to-end solutions.
Using these advanced technologies, better optimized cell line selection can expedite clone choice, while higher throughput screening and assessment, greater capacity to conduct parallel development, and automated cell line selection, cell culture, and downstream development can all have significant impacts on timelines.
Open access platforms
As well as investing in advanced technologies at individual facilities, another key learning from the COVID-19 pandemic was the tremendous value of collaboration. When organizations and countries work together toward a common goal, we can achieve much more than when we all just work in isolation.
Therefore, it is our vision that every vaccine can be made by building an open access platform with the most comprehensive capabilities and technologies in the global biologics industry. An ability to draw on more open access research knowledge and technical know-how should allow us all to integrate high-quality, consistent healthcare in all corners of the world, ensuring that the populations of all countries have fair and equal access to life-saving vaccines.
Faster bioprocessing
Once an effective vaccine has been developed and approved, significant challenges remain in manufacturing. This was particularly evident during the COVID-19 pandemic, when vaccine production chains struggled to meet global demand. It has been suggested that the main causes for supply disruptions and delays included an insufficient number of vaccine manufacturing facilities, a lack of tech-transfer capability, inefficient arrangement of production stakeholders, and critical shortages in raw materials.
Addressing these manufacturing challenges involves the development of scalable processes at biotech manufacturing facilities that have the capacity to produce the required volumes of vaccine. New modular and flexible manufacturing technologies, including single-use bioprocessing systems, bring important benefits. Compared with conventional stainless-steel bioreactor facilities, the use of multiple single-use bioreactors offers a highly flexible, cost-competitive manufacturing strategy, ideally suited to the fluid demands of the vaccine market. These systems can be rapidly deployed for scaling up and scaling out to meet changing demands and easily repurposed for different vaccine candidates.

Continuing the application of automation through to the end of manufacture, fill and finish services are an important added offering. GMP production capabilities with fully automated, fully programmable sterile fill systems for vials and prefilled syringes can offer a streamlined finish while minimizing waste and maximizing safety.
It is also vitally important that those facilities have secure and stable supply chains. Especially following widespread disruptions to supply chains in recent years, due to the COVID-19 pandemic and other geopolitical issues, ensuring that any facility has the necessary network to meet its supply chain requirements consistently and reliably has become a key consideration.
For recombinant protein vaccine developers, this includes access to effective GMP-grade adjuvants, which have been known to cause bottlenecks in production. Therefore, it is important for vaccine manufacturers to make sure they have a strong supply chain for these adjuvants, or the ability to produce their own.
Under pressure
As recently as five years ago, contract development and manufacturing organizations (CDMOs) were not commonly used for the production of vaccines. However, in the wake of COVID-19, the world’s vaccine manufacturing footprint has altered. While four leading vaccine development companies still account for over 80% of the global vaccine market, these organizations faced significant challenges in responding to the pandemic. Suddenly finding themselves with insufficient capacity to provide the huge volumes of vaccines required, and facing supply chain challenges caused by the pandemic, many of these organizations engaged CDMOs for the first time.
Due to their innate ability to be more agile and responsive to external pressures, CDMOs were able to ramp up capabilities where they were needed for the production of large quantities of vaccines in a timely manner. While biologics was once considered a relatively niche offering, over the past four years it has become a much more common service provided by an increasing number of CDMOs, as they have invested in new sites—or upgraded existing ones—to increase biotech capacities and reallocate resources.
The challenge has been to ensure that any new and improved sites commission their qualification and validation (CQV) activities and receive GMP and other relevant regulatory certifications from relevant authorities in a timely manner.

Many CDMOs—especially the larger ones—have also been in a position to leverage long-term relationships with suppliers to implement alternative strategies to address supply chain disruptions caused by the pandemic and other geopolitical issues. While vaccine development is essentially a matter of R&D, business relationships and networks cannot be ignored as they ensure the continuity of reliable supply chains.
Frontline armaments in humanity’s future battle against the unknown must be large-capacity biotech sites, equipped with the best available facilities, with automated high-throughput workflows and highly flexible, cost-competitive bioprocessing and manufacturing strategies. Broader uptake of these technologies will allow vaccination responses to be faster, more efficacious, and more cost-effective, shortening the time it takes for them to reach patients and enabling us to be better prepared for future health crises.
Our ultimate goal, of course, is to achieve CEPI’s aspirational 100-day timeline. We believe it can be done for recombinant protein vaccines.
Jason He, PhD, is CMC Head, WuXi Vaccines, in Blue Bell, PA.









